Abstract
Introduction: Haplo-identical donor transplant (HIDT) with post-transplant cyclophosphamide (pCY) has emerged as a potential life-saving treatment modality for patients with limited donor availability. Although HIDT using bone marrow grafts with reduced intensity conditioning regimen has shown promising results, the data on peripheral stem cells are limited. In addition, very little is known about outcomes of cytokine release syndrome (CRS) in this population. We aimed to compare outcomes of pCY graft vs. host disease (GVHD) prophylaxis between HIDT (group 1) and mismatched unrelated, matched unrelated and related transplant (group 2) using peripheral hematopoietic stem cells transplants (PHSCT).
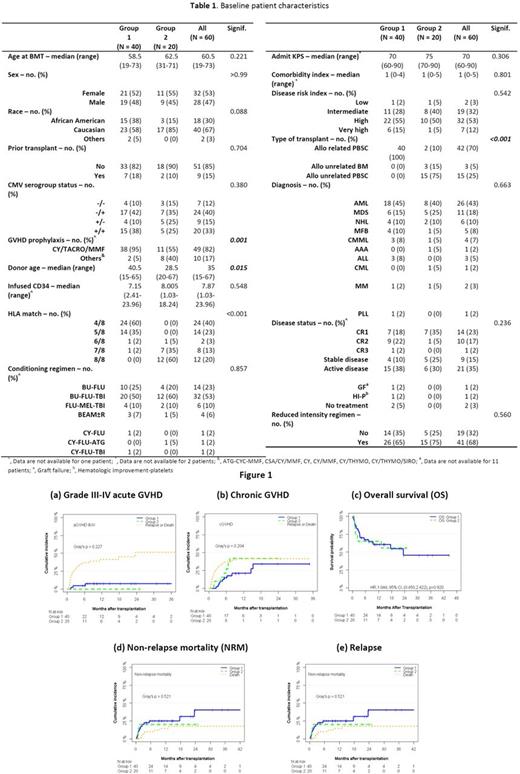
Methods: We retrospectively reviewed consecutive adult patients with hematologic malignancies who underwent HIDT (group 1), mismatched unrelated, matched unrelated and related PHSCT (group 2). All patients received pCY as GVHD prophylaxis either alone or in combination with other agents. The primary objectives were to determine rate of GVHD, non-relapse mortality (NRM), relapse rate, relapse free survival (RFS) and overall survival (OS) in both groups at 1-year.
Results: A total of 60 patients underwent peripheral blood stem cell transplant between January 2012 to October 2016. Forty patients received HIDT, whereas 10, 8 and 2 patients received mismatched unrelated, matched unrelated and related PHSCT, respectively. The median age of patients was 60.5 years (range, 19-73). AML was the most common diagnosis, followed by MDS and NHL. BU-FLU-TBI (53%) was the most common conditioning regimen used followed by BU-FLU (23%) and FLU-MEL-TBI (10%). The incidence of CRS was 89% in group 1. Grade 1, grade 2, grade 3 and grade 4 CRS was observed in 18 (50%), 9 (25%), 4 (11%) and 1 (3%) patients, respectively. Five patients required tocilizumab and 3 patients received systemic steroids for management of CRS. The median time to neutrophil engraftment was 18 days (range, 12-25) in group 1 and 17 days (range, 13-22) in group 2. The graft failure rate was 10% in each group.
The 1-year cumulative incidence of grade III-IV acute GVHD was 7.7% (95% CI, 1.9-19%) in group 1 and 0% in group 2. The 1-year cumulative incidence of chronic GVHD was 21.1% (95% CI, 9.6-35.6%) in group 1 and 41.7% (95% CI, 17.3-64.7%) in group 2. The 1-year cumulative incidence of NRM was 25.2% (95% CI, 12.9-39.5%) in group 1 and 20.0% (95% CI, 6.0-39.9%) in group 2, whereas RFS was 51.5% (95% CI, 37.99-70.06%) in group 1 and 56.8% (95% CI, 37.57-86.11%) in group 2. The 1-year relapse rate was 23.4% (95% CI, 11.3-38%) for group 1 and 23.1% (95% CI, 6.2-46.2%). The median follow-up of living patients was 14.4 months (95% CI, 10.43-23.7) in group 1 and 16.5 months (95% CI, 8.69-NR) in group 2. The 1-year OS was 60.6% (95% CI, 46.76-78.75%) in group 1, and 65% (95% CI, 47.12-89.66%) in group 2. Slightly higher rate of CMV reactivation was observed in group 1 (55% vs 40%, p=0.412), whereas rates of EBV reactivation, C. difficile colitis, invasive fungal and bacterial infections were similar in both groups. No differences in NRM, RFS, relapse rate and OS were found between both groups in multivariable analyses. No differences in GVHD, NRM and OS were noticed in patients with CRS. Disease recurrence and infections were the most common causes of death.
Conclusion: Our study demonstrates that pCY provides comparable rates of GVHD, relapse rate and OS in haplo-identical, mismatched unrelated, matched unrelated and related peripheral blood stem cell transplants. pCY can be used as GVHD prophylaxis to provide good post-transplant outcomes regardless of donor source.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal